![Image result for γ-Secretase Inhibitors BMS]()
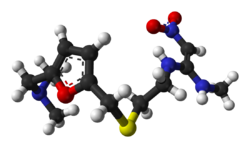
BMS 906024
cas 1401066-79-2
- MF C26H26F6N4O3
- MW 556.500
(2R,3S)-N-[(3S)-1-Methyl-2-oxo-5-phenyl-2,3-dihydro-1H-1,4-benzodiazepin-3-yl]-2,3-bis(3,3,3-trifluoropropyl)succinamide
Butanediamide, N1-((3S)-2,3-dihydro-1-methyl-2-oxo-5-phenyl-1H-1,4-benzodiazepin-3-yl)-2,3-bis(3,3,3-trifluorophenyl)-, (2R,3S)-
(2R,35)-N-((35)-l-Methyl-2-oxo-5-phenyl-2,3-dihydro-lH-l,4-benzodiazepin-3-yl)-3- (2,2,2-trifluoroethyl)-2-(3,3,3-trifluoropropyl)succinamide
![str2]()
Ashvinikumar Gavai
![Claude Quesnelle]()
Claude Quesnelle
Senior Research Investigator/Chemist at Bristol-Myers Squibb
![str2]()
RICHARD LEE
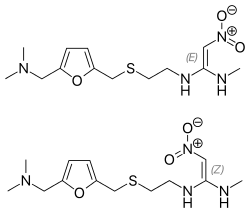
BMS-906024 is a novel, potent Notch receptor inhibitor . Cancers have a tendency to relapse or to become resistant to treatments that once worked. A family of proteins called Notch is implicated in that resistance and in cancer progression more generally. BMS-906024 is in Phase I clinical trials, both alone and in combination with other agents. Patients with colon, lung, breast, and other cancers are receiving intravenous doses of the compound to determine its safety and optimum dose ranges.
New Phase I drug structure by Bristol-Myers Squibb disclosed at the spring 2013 American Chemical Society meeting in New Orleans to treat breast, lung, and colon cancers and leukemia.[1] The drug works as an pan-Notch inhibitor. The structure is one of a set patented in 2012,[2] and it currently being studied in clinical trials.[3][4]
useful for the treatment of conditions related to the Notch pathway, such as cancer and other proliferative diseases.
Notch signaling has been implicated in a variety of cellular processes, such as cell fate specification, differentiation, proliferation, apoptosis, and angiogenesis. (Bray, Nature Reviews Molecular Cell Biology, 7:678-689 (2006); Fortini, Developmental Cell 16:633-647 (2009)). The Notch proteins are single-pass heterodimeric transmembrane molecules. The Notch family includes 4 receptors, NOTCH 1-4, which become activated upon binding to ligands from the DSL family (Delta-like 1, 3, 4 and Jagged 1 and 2).
The activation and maturation of NOTCH requires a series of processing steps, including a proteolytic cleavage step mediated by gamma secretase, a multiprotein complex containing Presenilin 1 or Presenilin 2, nicastrin, APH1, and PEN2. Once NOTCH is cleaved, NOTCH intracellular domain (NICD) is released from the membrane. The released NICD translocates to the nucleus, where it functions as a transcriptional activator in concert with CSL family members (RBPSUH, “suppressor of hairless”, and LAG1). NOTCH target genes include HES family members, such as HES- 1. HES- 1 functions as transcriptional repressors of genes such as HERP 1 (also known as HEY2), HERP2 (also known as HEY1), and HATH1 (also known as ATOH1).
The aberrant activation of the Notch pathway contributes to tumorigenesis. Activation of Notch signaling has been implicated in the pathogenesis of various solid tumors including ovarian, pancreatic, as well as breast cancer and hematologic tumors such as leukemias, lymphomas, and multiple myeloma. The role of Notch inhibition and its utility in the treatment of various solid and hematological tumors are described in Miele, L. et al, Current Cancer Drug Targets, 6:313-323 (2006); Bolos, V. et al, Endocrine Reviews, 28:339-363 (2007); Shih, I.-M. et al, Cancer Research, 67: 1879- 1882 (2007); Yamaguchi, N. et al., Cancer Research, 68: 1881-1888 (2008); Miele, L., Expert Review Anti-cancer Therapy, 8: 1 197-1201 (2008); Purow, B., Current Pharmaceutical Biotechnology, 10: 154-160 (2009); Nefedova, Y. et al, Drug Resistance Updates, 1 1 :210-218 (2008); Dufraine, J. et al, Oncogene, 27:5132-5137 (2008); and Jun, H.T. et al, Drug Development Research, 69:319-328 (2008).
There remains a need for compounds that are useful as Notch inhibitors and that have sufficient metabolic stability to provide efficacious levels of drug exposure. Further, there remains a need for compounds useful as Notch inhibitors that can be orally or intravenously administered to a patient.
U.S. Patent No. 7,053,084 Bl discloses succinoylamino benzodiazepine compounds useful for treating neurological disorders such as Alzheimer’s Disease. The reference discloses that these succinoylamino benzodiazepine compounds inhibit gamma secretase activity and the processing of amyloid precursor protein linked to the formation of neurological deposits of amyloid protein. The reference does not disclose the use of these compounds in the treatment of proliferative diseases such as cancer.
Applicants have found potent compounds that have activity as Notch inhibitors and have sufficient metabolic stability to provide efficacious levels of drug exposure upon intravenous or oral administration. These compounds are provided to be useful as pharmaceuticals with desirable stability, bioavailability, therapeutic index, and toxicity values that are important to their drugability.
![Image result for BMS 906024]()
![Image result for BMS 906024]()
![Image result for BMS 906024 synthesis]()
PAPER
![Abstract Image]()
Structure–activity relationships in a series of (2-oxo-1,4-benzodiazepin-3-yl)-succinamides identified highly potent inhibitors of γ-secretase mediated signaling of Notch1/2/3/4 receptors. On the basis of its robust in vivo efficacy at tolerated doses in Notch driven leukemia and solid tumor xenograft models, 12 (BMS-906024) was selected as a candidate for clinical evaluation.
Discovery of Clinical Candidate BMS-906024: A Potent Pan-Notch Inhibitor for the Treatment of Leukemia and Solid Tumors
Ashvinikumar V. Gavai*†, Claude Quesnelle†, Derek Norris†, Wen-Ching Han†, Patrice Gill†, Weifang Shan†, Aaron Balog†, Ke Chen§, Andrew Tebben†, Richard Rampulla†, Dauh-Rurng Wu†, Yingru Zhang†, Arvind Mathur†,Ronald White†, Anne Rose†, Haiqing Wang†, Zheng Yang†, Asoka Ranasinghe†, Celia D’Arienzo†, Victor Guarino†, Lan Xiao†, Ching Su†, Gerry Everlof†, Vinod Arora‡, Ding Ren Shen†, Mary Ellen Cvijic†, Krista Menard†, Mei-Li Wen†, Jere Meredith‡, George Trainor†, Louis J. Lombardo†, Richard Olson‡, Phil S. Baran§,John T. Hunt†, Gregory D. Vite†, Bruce S. Fischer†, Richard A. Westhouse†, and Francis Y. Lee†
†Bristol-Myers Squibb Research and Development, Princeton, New Jersey 08543, United States
‡Bristol-Myers Squibb Research and Development, 5 Research Parkway, Wallingford, Connecticut 06492, United States
§ Department of Chemistry, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, California 92037,United States
ACS Med. Chem. Lett., 2015, 6 (5), pp 523–527
(2R,3S)-N-((3S)-1-methyl-2-oxo-5-phenyl-2,3-dihydro-1H-1,4- benzodiazepin-3-yl)-2,3-bis(3,3,3-trifluoropropyl)succinamide
colorless solid: HPLC: RT = 9.60 min (HPLC Method D). Chiral LC/Analytical SFC conditions: Column: LuxCellulose-2 (0.46 x 25cm), Mobile phase: 10% methanol in CO2, Flow rate: 3 mL/min, wavelength: 220 nm; Temp.: 35C. RT = 9.21 min, Purity = 99.95%.
MS (ES): m/z = 557 [M+H]+ ;
1H NMR (400 MHz, DMSO-d6) 9.54 (1H, d, J = 7.28 Hz), 7.71 – 7.80 (1H, m), 7.68 (2H, d, J = 8.78 Hz), 7.50 – 7.62 (3H, m), 7.45 (2H, t, J = 7.28 Hz), 7.29 – 7.40 (2H, m), 7.15 (1H, s), 5.30 (1H, d, J = 7.28 Hz), 3.39 (3H, s), 2.74 – 2.86 (1H, m), 2.02 -2.32 (3H, m), 1.45 – 1.79 (4H, m);
[]D = -107.0° (5.73 mg/mL, DMSO).
Elemental analysis: Theoretical: C: 54.11%; H: 4.70%; N: 10.06%; Actual: C: 54.06%; H: 4.90%; N: 10.08%.
Karl Fisher Moisture: 0.48.
HPLC Method D: Sunfire C18 3.5um, 3.0x150mm column, solvent A: 5% acetonitrile – 95% water – 0.05% TFA, solvent B: 95% acetonitrile – 5% water – 0.05% TFA, flow=0.5 mL/min, gradient from 10%B to 100%B over 15min, 254 nm detector.
Patent
http://www.google.co.in/patents/WO2012129353A1?cl=en
Example 1
(2R,35)-N-((35′)-l-Methyl-2-oxo-5-phenyl-2,3-dihydro-lH-l,4-benzodiazepin-3-yl)-2,3- b -trifluoropropy l)succinamide
Preparation 1A: tert-Butyl 5, -trifluoropentanoate
![Figure imgf000065_0002]()
[00219] To a stirred solution of 5,5,5-trifluoropentanoic acid (5 g, 32.0 mmol) in THF (30 mL) and hexane (30 mL) at 0 °C, was added tert-butyl 2,2,2-trichloroacetimidate (11.46 mL, 64.1 mmol). The mixture was stirred for 15 min at 0 °C. Boron trifluoride etherate (0.406 mL, 3.20 mmol) was added and the reaction mixture was allowed to warm to room temperature overnight. To the clear reaction mixture was added solid aHC03 (5 g) and stirred for 30 min. The mixture was filtered through MgS04 and washed with hexanes (200 mL). The solution was allowed to rest for 45 min, and the resulting solid material was removed by filtering on the same MgS04 filter again, washed with hexanes (100 mL) and concentrated under reduced pressure without heat. The volume was reduced to about 30 mL, filtered through a clean fritted funnel, washed with hexane (5 mL), and then concentrated under reduced pressure without heat. The resulting neat oil was filtered through a 0.45μηι nylon membrane filter disk to provide tert-butyl 5,5,5- trifluoropentanoate (6.6 g, 31.4 mmol 98% yield) as a colorless oil: XH NMR (400 MHz, CDC13) δ ppm 1.38 (s, 9 H) 1.74-1.83 (m, 2 H) 2.00-2.13 (m, 2 H) 2.24 (t, J=7.28 Hz, 2 H).
Preparation IB: (45)-4-(Propan-2- l)-3-(5,5,5-trifluoropentanoyl)-l,3-oxazolidin-2-one
![Figure imgf000066_0001]()
[00220] To a stirred solution of 5,5,5-trifluoropentanoic acid (5.04 g, 32.3 mmol) in DCM (50 mL) and DMF (3 drops) was added oxalyl chloride (3.4 mL, 38.8 mmol) dropwise over 5 min and the solution was stirred until all bubbling subsided. The reaction mixture was concentrated under reduced pressure to give pale yellow oil. To a separate flask charged with a solution of (45)-4-(propan-2-yl)-l,3-oxazolidin-2-one (4.18 g, 32.4 mmol) in THF (100 mL) at -78 °C was added n-BuLi (2.5M in hexane) (13.0 mL, 32.5 mmol) dropwise via syringe over 5 min. After stirring for 10 min, the above acid chloride dissolved in THF (20 mL) was added via cannula over 15 min. The reaction mixture was warmed to 0 °C, and was allowed to warm to room temperature as the bath warmed and stirred overnight. To the reaction mixture was added saturated NH4CI, and then extracted with EtOAc (2x). The combined organics were washed with brine, dried (Na2S04), filtered and concentrated under reduced pressure. The crude material was purified by flash chromatography (Teledyne ISCO CombiFlash Rf, 5% to 60% solvent A/B=hexanes/EtOAc, REDISEP® S1O2 120g). Concentration of appropriate fractions provided Preparation IB (7.39 g, 86%) as a colorless oil: XH NMR (400 MHz, CDC13) δ ppm 4.44 (1 H, dt, J=8.31, 3.53 Hz), 4.30 (1 H, t, J=8.69 Hz), 4.23 (1 H, dd, J=9.06, 3.02 Hz), 2.98-3.08 (2 H, m), 2.32-2.44 (1 H, m, J=13.91, 7.02, 7.02, 4.03 Hz), 2.13-2.25 (2 H, m), 1.88-2.00 (2 H, m), 0.93 (3 H, d, J=7.05 Hz), 0.88 (3 H, d, J=6.80 Hz). Preparation 1C: (25′,3R)-tert-Butyl 6,6,6-trifluoro-3-((5)-4-isopropyl-2-oxooxazolidine- 3 -carbonyl)-2-(3 ,3,3 -trifluoropropyl)hexanoate, and
Preparation ID: (2R,3R)-tert-Butyl 6,6,6-trifluoro-3-((5)-4-isopropyl-2-oxooxazolidine- 3 -carbonyl)- -(3 ,3 ,3 -trifluoropropyl)hexanoate
(1 C) (1 D)
[00221] To a cold (-78 °C), stirred solution of diisopropylamine (5.3 mL, 37.2 mmol) in THF (59 mL) under nitrogen atmosphere was added n-BuLi (2.5M in hexane) (14.7 mL, 36.8 mmol), then warmed to 0 °C to give a 0.5M solution of LDA. A separate vessel was charged with Preparation IB (2.45 g, 9.17 mmol), the material was azeotroped twice with benzene (the RotoVap air inlet was fitted with nitrogen inlet to completely exclude humidity) then toluene (15.3 mL) was added. This solution was added to a flask containing dry lithium chloride (1.96 g, 46.2 mmol). To the resultant mixture, cooled to -78 °C, was added LDA solution (21.0 mL, 10.5 mmol) and stirred at -78 °C for 10 min, warmed to 0 °C for 10 min then recooled to -78 °C. To a separate reaction vessel containing Preparation 1A (3.41 g, 16.07 mmol), also azeotroped twice with benzene, was added toluene (15.3 mL), cooled to -78 °C and LDA (37.0 mL, 18.5 mmol) was added, the resulting solution was stirred at -78° for 25 min. At this time the enolate derived from the ester was transferred via cannula into the solution of the oxazolidinone enolate, stirred at -78 °C for an additional 5 min at which time the septum was removed and solid powdered bis(2-ethylhexanoyloxy)copper (9.02 g, 25.8 mmol) was rapidly added to the reaction vessel and the septum replaced. The vessel was immediately removed from the cold bath and immersed into a warm water bath (40 °C) with rapid swirling with a concomitant color change from the initial turquoise to brown. The reaction mixture was stirred for 20 min, was poured into 5% aqueous NH4OH (360 mL) and extracted with EtOAc (2x). The combined organics were washed with brine, dried (Na2S04), filtered and concentrated under reduced pressure. The residue was purified by flash chromatography (Teledyne ISCO CombiFlash Rf, 0% to 60% solvent A/B=hexanes/EtOAc, REDISEP® S1O2 120g). Concentration of appropriate fractions provided Preparation 1C (2.87 g, 66%) as pale yellow viscous oil. XH NMR showed the product was a 1.6: 1 mixture of diastereoisomers 1C: 1D as determined by the integration of the multiplets at 2.74 & 2.84 ppm: XH NMR (400 MHz, CDC13) δ ppm 4.43-4.54 (2 H, m), 4.23-4.35 (5 H, m), 4.01 (1 H, ddd, J=9.54, 6.27, 3.51 Hz), 2.84 (1 H, ddd, J=9.41, 7.28, 3.64 Hz), 2.74 (1 H, ddd, J=10.29, 6.27, 4.02 Hz), 2.37-2.48 (2 H, m, J=10.38, 6.98, 6.98, 3.51, 3.51 Hz), 2.20-2.37 (3 H, m), 1.92-2.20 (8 H, m), 1.64-1.91 (5 H, m), 1.47 (18 H, s), 0.88-0.98 (12 H, m). Preparation IE: (2R,35)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid, and
Preparation IF: (2R,3R)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid
(1 E) (1 F)
[00222] To a cool (0 °C), stirred solution of Preparation 1C and ID (4.54 g, 9.51 mmol) in THF (140 mL) and water (42 mL) was sequentially added hydrogen peroxide (30% in water) (10.3 g, 91 mmol) and LiOH (685.3 mg, 28.6 mmol) and the mixture was stirred for 1 hr. At this time the reaction vessel was removed from the cold bath and then stirred for 1.5 hr. The reaction was judged complete by HPLC. To the reaction mixture was added saturated NaHC03 (45 mL) and saturated a2S03(15 mL), and then partially concentrated under reduced pressure. The resulting crude solution was extracted with DCM (3x). The aqueous phase was acidified to pH~l-2 with IN HC1, extracted with DCM (3x) and EtOAc (lx). The combined organics were washed with brine, dried (Na2S04), filtered and concentrated under reduced pressure to provide a mixture of Preparation IE and IF (3.00 g, 86%) as colorless oil: XH NMR (400 MHz, CDC13) δ ppm 2.76-2.84 (1 H, m, diastereoisomer 2), 2.64-2.76 (3 H, m), 2.04-2.35 (8 H, m), 1.88-2.00 (4 H, m), 1.71-1.83 (4 H, m), 1.48 (9 H, s, diastereoisomer 1), 1.46 (9 H, s, diastereoisomer 2); XH NMR showed a 1.7: 1 mixture of 1E: 1F by integration of the peaks for the ?-butyl groups.
Preparation IE: (2R,35)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid, and
Preparation IF: (2R,3R)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid
(1 E) (1 F)
[00223] To a cold (-78 °C), stirred solution of diisopropylamine (1.7 mL, 11.93 mmol) in THF (19 mL) under nitrogen atmosphere was added n-BuLi (2.5M in hexanes) (4.8 mL, 12.00 mmol). The mixture was stirred for 5 min and then warmed to 0 °C. In a separate vessel, to a cold (-78 °C) stirred solution of the mixture of Preparation IE and IF (1.99 g, 5.43 mmol) in THF (18 mL) was added the LDA solution prepared above via cannula slowly over 25 min. The mixture was stirred for 15 min, then warmed to room temperature (placed in a 24 °C water bath) for 15 min, and then again cooled to -78 °C for 15 min. To the reaction mixture was added Et2AlCl (1M in hexane) (11.4 mL, 1 1.40 mmol) via syringe, stirred for 10 min, warmed to room temperature for 15 min and then cooled back to -78 °C for 15 min. Methanol (25 mL) was rapidly added, swirled vigorously while warming to room temperature, then concentrated to ~l/4 original volume. The mixture was dissolved in EtOAc and washed with IN HCl (50 mL) and ice (75 g). The aqueous phase was separated, extracted with EtOAc (2x). The combined organics were washed with a mixture of KF (2.85g in 75 mL water) and IN HCl (13 mL) [resulting solution pH 3-4], then with brine, dried (Na2S04), filtered and concentrated under reduced pressure to give a 9: 1 (IE: IF) enriched diastereoisomeric mixture (as determined by XH NMR) of Preparation IE and Preparation IF (2.13 g, >99%) as a pale yellow viscous oil: XH NMR (400 MHz, CDC13) δ ppm 2.64-2.76 (2 H, m), 2.04-2.35 (4 H, m), 1.88-2.00 (2 H, m), 1.71-1.83 (2 H, m), 1.48 (9 H, s). Preparation 1 G: (35)-3 -Amino- 1 -methyl-5-phenyl- 1 ,3 -dihydro-2H- 1 ,4-benzodiazepin-2- one, and
Preparation 1H: (3R)-3 -Amino- 1 -methyl-5-phenyl- 1 ,3-dihydro-2H- 1 ,4-benzodiazepin-2- one
(1G) (1 H)
[00224] Racemic 3-amino-l-methyl-5-phenyl-l,3-dihydro-2H-l,4-benzodiazepin-2- one (Rittle, K.E. et al, Tetrahedron Letters, 28(5):521-522 (1987)) was prepared according to the literature procedure. The enantiomers were separated under chiral-SFC conditions using the following method: CHIRALPAK® AS-H 5×25; Mobile phase: 30% MeOH+ 0.1% DEA in C02; Flow rate: 280 mL/min; Pressure: 100 bar; Temperature: 35 °C.
[00225] Obtained the S-enantiomer (Preparation 1G): HPLC: RT=1.75 min (30% MeOH + 0.1% DEA in C02 on CHIRALPAK® AS-H 4.6×250 mm, 3 mL/min, 35 °C, 100 bar, 230 nm, ΙΟμΙ injection); ¾ NMR (400 MHz, CDC13) δ ppm 7.58-7.63 (2 H, m), 7.55 (1 H, ddd, J=8.50, 7.1 1, 1.76 Hz), 7.40-7.47 (1 H, m), 7.34-7.40 (3 H, m), 7.31 (1 H, dd, J=7.81, 1.51 Hz), 7.14-7.22 (1 H, m), 4.46 (1 H, s), 3.44 (3 H, s), 3.42 (2 H, s); [a]D= -155° (c=1.9, MeOH) (Lit. Rittle, K.E. et al, Tetrahedron Letters, 28(5):521-522 (1987): [a]D=-236°).
[00226] Also obtained the R-enantiomer (Preparation 1H): HPLC: RT=1.71 min; [a]D=+165° (c=2.1, MeOH) (Lit [a]D= +227°).
Alternate procedure to make Preparation 1 G:
Preparation 1G»CSA salt: (35)-3-Amino-l-methyl-5-phenyl-l,3-dihydro-2H-l,4- benzodiazepin-2-one, (15)-(+)-10-camphorsulfonic acid salt
[00227] Preparation lG’CSA was prepared from racemic 3-amino-l-methyl-5-phenyl- l,3-dihydro-2H-l,4-benzodiazepin-2-one (9.98g, 37.6 mmol) (prepared according to the literature as shown above) according to the literature procedure (Reider, P.J. et al, J. Org. Chem., 52:955-957 (1987)). Preparation lG’CSA (16.91g, 99%) was obtained as a colorless solid: Optical Rotation: [a]D = -26.99° (c=l, H20) (Lit. [a]D = -27.8° (c=l,
H20))
Preparation II: tert-Butyl (25,,3R)-6,6,6-trifluoro-3-(((35)-l-methyl-2-oxo-5-phenyl-2,3- dihydro- 1 H- 1 ,4-benzodiazepin-3 -yl)carbamoyl)-2-(3 ,3 ,3 -trifluoropropyl)hexanoate, and Preparation 1J: tert-Butyl (2R,3R)-6,6,6-trifluoro-3-(((35)-l-methyl-2-oxo-5-phenyl-2,3- dihydro- 1 H- 1 ,4-benzodiazepin-3 -yl)carbamoyl)-2-(3 ,3 ,3-trifluoropropyl)hexanoate
(11) (U)
[00228] To a stirred solution of Preparation 1G (1.45 g, 5.47 mmol) and a 9: 1 mixture of Preparation IE and IF (1.989 g, 5.43 mmol) in DMF (19 mL) was added O- benzotriazol-l-yl-N,N,N’,N’-tetra-methyluronium tetrafluoroborate (1.79 g, 5.57 mmol) and triethylamine (3.0 mL, 21.52 mmol) and stirred overnight. The reaction was judged complete by LCMS. The reaction mixture was poured into water (125 mL) and the precipitated solid was collected by filtration, washed with water and air dried to provide an 8: 1 mixture of Preparation II and Preparation 1J (2.95 g, 89%) as a cream solid: MS (ES): m/z= 614 [M+H]+;XH NMR (400 MHz, CDC13) δ ppm 7.55-7.65 (3 H, m), 7.44- 7.52 (2 H, m), 7.35-7.45 (4 H, m), 5.52 (1 H, d, J=8.03 Hz), 3.48 (3 H, s), 2.63 (2 H, ddd, J=9.35, 3.95, 3.76 Hz), 2.14-2.25 (4 H, m), 1.90-2.03 (3 H, m), 1.69-1.82 (1 H, m), 1.51 (9 H, s).
Preparation IK: (25,,3R)-6,6,6-Trifluoro-3-(((35)-l-methyl-2-oxo-5-phenyl-2,3-dihydro- lH-l,4-benzodiazepin-3-yl)carbamoyl)-2-(3,3,3-trifluoropropyl)hexanoic acid, and
Preparation 1L: (2R,3R)-6,6,6-Trifluoro-3-(((35)-l-methyl-2-oxo-5-phenyl-2,3-dihydro- 1 H- 1 ,4-
(1 K) (1 L)
[00229] To a cool (0 °C), stirred solution of the above mixture of Preparation II and Preparation 1 J (2.95 g, 4.81 mmol) in DCM (20 mL) was added TFA (20 mL, 260 mmol). The reaction mixture was stirred for lhr, then allowed to warm to room temperature and stirred for 2.5 hr. The reaction was judged complete by LCMS. The reaction mixture was diluted with toluene (50 mL) and concentrated under reduced pressure. The residue mixture was redissolved in toluene (50 mL) and concentrated under reduced pressure then dried under high vacuum. The crude product was dissolved in DCM, S1O2 (15g) was added, concentrated, then was purified by flash chromatography (Teledyne ISCO CombiFlash Rf, 0% to 45% solvent A/B=DCM/EtOAc, REDISEP® S1O2 80g). Concentration of appropriate fractions provided a mixture of Preparation IK and Preparation 1L (2.00 g, 75%) as a cream solid: HPLC: RT=2.770 min
(CHROMOLITH® SpeedROD 4.6 x 50 mm (4 min grad) eluting with 10-90% aqueous MeOH over 4 minutes containing 0.1% TFA, 4 mL/min, monitoring at 254 nm); MS (ES): m/z= 558 [M+H]+; XH NMR (400 MHz, CDC13) δ ppm 8.32 (1 H, d, J=8.03 Hz), 7.65-7.71 (1 H, m), 7.50-7.60 (3 H, m), 7.41-7.49 (2 H, m), 7.39 (1 H, dd, J=7.91, 1.63 Hz), 7.23-7.35 (2 H, m), 5.59 (1 H, d, J=8.03 Hz), 3.51 (3 H, s), 2.81 (1 H, ddd, J=10.54, 6.90, 3.64 Hz), 2.67-2.76 (1 H, m), 2.22-2.33 (3 H, m), 1.99-2.12 (3 H, m), 1.85-1.94 (1 H, m), 1.79 (1 H, ddd, J=13.87, 7.84, 3.64 Hz). Example 1 :
[00230] To a stirred solution of an 8: 1 mixture of Preparation IK and Preparation 1L (3.46 g, 6.21 mmol) in DMF (25 mL) under nitrogen atmosphere was added ammonium chloride (3.32 g, 62.1 mmol), EDC (3.55 g, 18.52 mmol), HOBT (2.85 g, 18.61 mmol), and triethyl amine (16 mL, 1 15 mmol) and stirred overnight. The reaction was judged complete by LCMS. The reaction mixture was poured into water (200 mL) with vigorous swirling and then allowed to sit. The solid was collected by filtration, washed with water, allowed to dry to afford 3.6 g colorless solid. The solid was purified by preparative SFC chromatography (Lux-Cellulose-2 (3x25cm), 8% methanol in CO2, 140ml/min @220nm and 35 °C; Sample: 3.6g in 50cc methanol, conc.=70mg/ml, Stack injection:
0.5cc/9.2min). Fractions containing product were concentrated, dried overnight under vacuum. Obtained Example 1 (2.74 g, 79%) as a colorless solid (Crystal Form -1): HPLC: RT=9.601 min (H20/CH3CN with TFA, Sunfire CI 8 3.5um, 4.6x150mm, 4.6x150mm, gradient = 15 min, wavelength = 220 and 254 nm). MS (ES): m/z= 557 [M+H]+; XH NMR (400 MHz, DMSO-d6) δ ppm 9.54 (1 H, d, J=7.28 Hz), 7.71-7.80 (1 H, m), 7.68 (2 H, d, J=8.78 Hz), 7.50-7.62 (3 H, m), 7.45 (2 H, t, J=7.28 Hz), 7.29-7.40 (2 H, m), 7.15 (1 H, br. s.), 5.30 (1 H, d, J=7.28 Hz), 3.39 (3 H, s), 2.74-2.86 (1 H, m), 2.02-2.32 (3 H, m), 1.45-1.79 (4 H, m); [a]D = -107.0° (5.73 mg/mL, DMSO).
[00231] Crystal Form A-2 was prepared by adding approximately 1 mg of Example 1 to approximately 0.7 mL of acetone/acetonitrile/water solution (2:2: 1). A mixture of colorless needles and thin blades crystals were obtained after one day of slow evaporation of the solution at room temperature. The thin blade crystals were separated to provide crystal Form A-2.
[00232] Crystal Form EA-3 was prepared by adding approximately 1 mg of Example 1 to approximately 0.7 mL of ethyl acetate/heptane solution (1 : 1). Colorless blade crystals were obtained after three days of slow evaporation of the solution at room temperature.
[00233] Crystal Form THF-2 was obtained by adding approximately 5 mg of Example 1 to approximately 0.7 mL of THF/water solution (4: 1). Colorless blade-like crystals were obtained after one day of solvent evaporation at room temperature.
Alternate Procedure to Make Example 1 : Preparation 1M: 3,3,3-Trifluoropropyl trifluoromethanesulfonate
[00234] To a cold (-25 °C), stirred solution of 2,6-lutidine (18.38 mL, 158 mmol) in CH2CI2 (120 mL) was added Tf20 (24.88 mL, 147 mmol) over 3 min, and stirred for 5 min. To the reaction mixture was added 3,3,3-trifluoropropan-l-ol (12 g, 105 mmol) over an interval of 3 min. After 2 hr, the reaction mixture was warmed to room temperature and stirred for 1 hr. The reaction mixture was concentrated to half volume, then purified by loading directly on silica gel column (330g ISCO) and eluted with CH2C12. Obtained Preparation 1M (13.74 g, 53%) as a colorless oil. XH NMR (400 MHz, CDCI3) δ ppm 4.71 (2 H, t, J=6.15 Hz), 2.49-2.86 (2 H, m).
Preparation IN: (45)-4-Benzyl- -(5,5,5-trifluoropentanoyl)-l,3-oxazolidin-2-one
[00235] Preparation IN was prepared from 5,5,5-trifluoropentanoic acid (3.35 g, 21.46 mmol) and (45)-4-benzyl-l,3-oxazolidin-2-one (3.80 g, 21.46 mmol) by the general methods shown for Preparation IB. Preparation IN (5.67 g, 84%) was obtained as a colorless viscous oil: XH NMR (400 MHz, CDC13) δ ppm 7.32-7.39 (2 H, m), 7.30 (1 H, d, J=7.05 Hz), 7.18-7.25 (2 H, m), 4.64-4.74 (1 H, m), 4.17-4.27 (2 H, m), 3.31 (1 H, dd, J=13.35, 3.27 Hz), 3.00-3.1 1 (2 H, m), 2.79 (1 H, dd, J=13.35, 9.57 Hz), 2.16-2.28 (2 H, m), 1.93-2.04 (2 H, m).
Preparation 10: tert-Butyl (3R)-3-(((45)-4-benzyl-2-oxo-l,3-oxazolidin-3-yl)carbonyl)- 6,6,6-trifluorohexanoate
![Figure imgf000075_0001]()
[00236] To a cold (-78 °C), stirred solution of Preparation IN (3.03 g, 9.61 mmol) in THF (20 mL) was added NaHMDS (1.0M in THF) (10.6 mL, 10.60 mmol) under nitrogen atmosphere. After 2 hours, tert-butyl 2-bromoacetate (5.62 g, 28.8 mmol) was added neat via syringe at -78 °C and stirring was maintained at the same temperature. After 6 hours, the reaction mixture was warmed to room temperature. The reaction mixture was partitioned between saturated NH4C1 and EtOAc. The organic phase was separated, and the aqueous was extracted with EtOAc (3x). The combined organics were washed with brine, dried (Na2S04), filtered and concentrated under reduced pressure. The residue was purified by flash chromatography (Teledyne ISCO CombiFlash Rf, 5% to 100% solvent A/B=hexanes/EtO Ac, REDISEP® Si02 120g). Concentration of appropriate fractions provided Preparation 10 (2.79 g, 67.6%) as a colorless viscous oil: XH NMR (400 MHz, CDC13) δ ppm 7.34 (2 H, d, J=7.30 Hz), 7.24-7.32 (3 H, m), 4.62- 4.75 (1 H, m, J=10.17, 6.89, 3.43, 3.43 Hz), 4.15-4.25 (3 H, m), 3.35 (1 H, dd, J=13.60, 3.27 Hz), 2.84 (1 H, dd, J=16.62, 9.57 Hz), 2.75 (1 H, dd, J=13.35, 10.07 Hz), 2.47 (1 H, dd, J=16.62, 4.78 Hz), 2.1 1-2.23 (2 H, m), 1.90-2.02 (1 H, m), 1.72-1.84 (1 H, m), 1.44 (9 H, s). -2-(2-tert-Butoxy-2-oxoethyl)-5,5,5-trifluoropentanoic acid
![Figure imgf000075_0002]()
[00237] Preparation IP was prepared from Preparation 10 (2.79 g, 6.50 mmol) by the general methods shown for Preparation IE. Preparation IP (1.45 g, 83%) was obtained as a colorless oil: XH NMR (400 MHz, CDC13) δ ppm 2.83-2.95 (1 H, m), 2.62-2.74 (1 H, m), 2.45 (1 H, dd, J=16.62, 5.79 Hz), 2.15-2.27 (2 H, m), 1.88-2.00 (1 H, m), 1.75-1.88 (1 H, m), 1.45 (9 H, s). Preparation IE: (2R,35′)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid, and
Preparation IF: (2R,3R)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid
(1 E) (1 F)
[00238] To a cold (-78 °C), stirred solution of Preparation IP (5.44 g, 20.13 mmol) in THF (60 mL) was slowly added LDA (24.60 mL, 44.3 mmol) over 7 min. After stirring for 2 hr, Preparation 1M (6.44 g, 26.2 mmol) was added to the reaction mixture over 3 min. After 45 min, the reaction mixture was warmed to -25 °C bath (ice/MeOH/dry ice) for 1 hr, and then warmed to 0 °C. After 45 min, Preparation 1M (lg) was added and the reaction mixture was stirred for 20 min. The reaction was quenched with water and IN NaOH and was extracted with (¾(¾. The organic layer was again extracted with IN NaOH (2x) and the aqueous layers were combined. The aqueous layer was cooled in ice/water bath and then acidified with concentrated HCl to pH 2. Next, the aqueous layer was extracted with EtOAc. The combined organics were washed with brine, dried over anhydrous sodium sulphate, and concentrated under reduced pressure. The residue was dried under high vacuum to provide a 1 :5 (IE: IF) mixture (as determined by XH NMR) of Preparation IE and Preparation IF (5.925 g, 80%) as a pale yellow solid. XH NMR (500 MHz, CDC13) 8 ppm 2.81 (1 H, ddd, J=10.17, 6.32, 3.85 Hz), 2.63-2.76 (1 H, m), 2.02- 2.33 (4 H, m), 1.86-1.99 (2 H, m), 1.68-1.85 (2 H, m), 1.47 (9 H, s).
Preparation IE: (2R,35)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid, and
Preparation IF: (2R,3R)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid
(1 E) (1 F)
[00239] A mixture of Preparation IE and Preparation IF (64 mg, 1.758 mmol) was taken in THF (6 mL) to give a colorless solution which was cooled to -78 °C. Then, LDA (2.149 mL, 3.87 mmol) (1.8M in heptane/THF/ethylbenzene) was slowly added to the reaction mixture over 10 min. After stirring for 15 min the reaction mixture was placed in a room temperature water bath. After 15 min the reaction mixture was placed back in -78 °C bath and then diethylaluminum chloride (3.87 mL, 3.87 mmol) (1M in hexane) was added slowly over 5 min. The reaction mixture was stirred at -78 °C. After 15 min the reaction mixture was placed in a room temperature water bath for 10 min and then cooled back to -78 °C bath. After 15 min the reaction was quenched with MeOH (8 mL, 198 mmol), removed from the -78 °C bath and concentrated. To the reaction mixture was added ice and HC1 (16 mL, 16.00 mmol), followed by extraction with EtOAc (2x). The organic layer was washed with potassium fluoride (920 mg, 15.84 mmol) (in 25 mL FLO) and HC1 (4.5 mL, 4.50 mmol). The organics were dried over anhydrous magnesium sulphate and concentrated under reduced pressure to provide a 9: 1 (IE: IF) enriched mixture of Preparation IE and Preparation IF (540 mg, 1.583 mmol, 90% yield) as light yellow/orange solid. ¾ NMR (400 MHz, CDC13) δ ppm 2.64-2.76 (2 H, m), 2.04-2.35 (4 H, m), 1.88-2.00 (2 H, m), 1.71-1.83 (2 H, m), 1.48 (9 H, s). It was converted to Example 1 by the sequence of reactions as outlined above.
Alternate procedure to make Preparation IE:
Preparation 1Q: (2R,35)- -Benzyl 4-tert-butyl 2,3-bis(3,3,3-trifluoropropyl)succinate
![Figure imgf000077_0002]()
(1Q) [00240] A clean and dry 5 L four neck round bottom flask equipped with mechanical stirring, thermometer socket and nitrogen bubbler at room temperature was charged with Ν,Ν-dimethyl formamide (2.07 L), a 1.2: 1 mixture of Preparation IE and Preparation IF (207 g, 0.5651 moles), potassium carbonate (1 17.1 g, 0.8476 moles) followed by benzyl bromide (116 g, 0.6781 moles) over 15-20 min. The reaction mixture was stirred for 2-3 hr. After completion of the reaction, the reaction mixture was concentrated to dryness at 50-55 °C under vacuum. Ethyl acetate (3.1 L, 30 Vol.) was charged into the concentrated reaction mass and then washed with water (2.07 L), brine (0.6 L) then dried over anhydrous sodium sulfate (207 g), filtered and concentrated to dryness at 40-45 °C under vacuum. The residue was dissolved in dichloromethane (1.035 L, 5 vol.) and then absorbed onto silica gel (60-120) (607 g, 3.0 w/w), then was purified with column chromatography using petroleum ether and ethyl acetate as solvents. After pooling several batches, Preparation 1Q (235 g) was obtained. HPLC purity: 99.77%, Preparation IE: (2R,35)-3-(tert-Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid
![Figure imgf000078_0001]()
[00241] A clean and dry 2 L autoclave was charged with methanol (540 mL) and was purged with nitrogen for 5-10 minutes. To the autoclave was added 10% palladium on carbon (12 g, 20%), purged with nitrogen once again for 5-10 min then was charged with Preparation 1Q (60g, 0.1315 moles), the autoclave was flushed with methanol (60mL) and stirred for 4-6 hr at 20-25 °C under 5Kg hydrogen pressure. After completion of the reaction, the reaction mass was filtered through CELITE®, washed with methanol (180 mL), dried with anhydrous sodium sulfate (60 g), filtered and concentrated to dryness at 45-50 °C under vacuum. Obtained Preparation IE (45.8 g, 95%) as a colorless solid: HPLC purity: 98.9%.
Alternate procedure to make Preparation IE: Preparation IE: (2R,35)-3-(te^Butoxycarbonyl)-6,6,6-trifluoro-2-(3,3,3- trifluoropropyl)hexanoic acid
[00242] Preparation IE was prepared in a procedure identical as above from a mixture of Preparations IE and IF (200g, 0.5460 moles) using LDA (1.8 M solution in THF, ethyl benzene and heptane) (698mL, 2.3equiv.) and diethyl aluminum chloride (1.0 M solution in hexane) (1256mL, 2.3equiv) in THF (2.0L). After workup as explained above, the resulting residue was treated as follows: The crude material was added to a 2L four neck round bottom flask, followed by the addition of MTBE (1.0L) charged below 30 °C. The resulting mixture was stirred for 5-10 minutes to obtain a clear solution.
Hexanes (600mL) was charged to the reaction mixture at a temperature below 30 °C. The reaction mixture was stirred for 10 min. Next, tert-butylamine (43.8g, l. leq) was charged slowly over a period of 15 minutes below 30 °C. This addition was observed to be exothermic. The reaction mixture was stirred for 2 hrs below 30 °C and filtered. The solid material was washed with 5:3 MTBE: hexane (200mL), the filtrate was
concentrated and transferred to an amber color bottle. The filtered solid was dissolved in dichloromethane (2.0L), washed with IN HC1 (2.0), the organic layer was washed with brine (1.0L x 2), then was concentrated under reduced pressure below 45 °C. This material was found to be 91.12% pure. The material was repurified by the above t- butylamine crystallization purification procedure. Obtained Preparation IE (78 g, 39%): HPLC purity: 99.54%.
Alternate procedure to make Example 1 :
Preparation II: tert-Butyl (25,,3R)-6,6,6-trifluoro-3-(((35)-l-methyl-2-oxo-5-phenyl-2,3- dihydro- 1 H- 1 ,4-benzodiazepin-3 -yl)carbamoyl)-2-(3 ,3 ,3 -trifluoropropyl)hexanoate
![Figure imgf000080_0001]()
[00243] A clean and dry 2 L four neck round bottom flask equipped with mechanical stirring, thermometer socket and nitrogen bubbler was charged with N,N- dimethylformamide (457 mL), Preparation IE (45.7g, 0.1248moles) and Preparation lG’CSA (62.08g, 0.1248moles) under nitrogen atmosphere at 20-25 °C. The reaction mixture was stirred for 15-20 minutes to make clear solution at 20-25 °C. To the reaction mixture was added TBTU (48.16g, 0.1498 moles) at 20-25 °C followed by triethylamine (50.51g, 0.4992 moles) over 15-20 minutes at 20-25 °C. The reaction mixture was stirred for 60-120 minutes at 20-25 °C under nitrogen atmosphere. After completion of the reaction, the reaction was quenched into water (1.37L, 30 Vol.) at 20-25 °C under stirring. The reaction mixture was stirred for 30 minutes at 20-25 °C. The reaction mixture was filtered and washed with water (228 mL). The resulting solid material was dissolved in ethyl acetate (457 mL), washed with water (2×137 mL), brine (137 mL), and then dried with anhydrous sodium sulfate (45.7g). Activated charcoal (9.14 g, 20%) was charged into the reaction mixture and stirred for 30 minutes. The mixture was filtered through CELITE® bed and 1 micron filter cloth, washed charcoal bed with ethyl acetate (137 mL), concentrated to 1.0 Vol. stage and then petroleum ether (457 mL, 10 Vol.) was charged and stirred for 30 minutes at 20-25 °C. The solid was collected by filtration, washed with petroleum ether (137 mL) and then dried under vacuum at 40-45 °C for 8 hr until loss on drying was less than 3.0%. Obtained Preparation II (65.2 g, 85%): HPLC purity: 98.26%.
Preparation IK: (25,,3R)-6,6,6-Trifluoro-3-(((35)-l-methyl-2-oxo-5-phenyl-2,3-dihydro- 1 H- 1 ,4-benzodiazepin-3 -yl)carbamoyl)-2-(3 ,3 ,3 -trifluoropropyl)hexanoic acid
![Figure imgf000081_0001]()
[00244] A clean and dry 3 L four neck round bottom flask equipped with mechanical stirring, thermometer socket and nitrogen bubbler was charged with dichloromethane (980 mL) under nitrogen atmosphere followed by Preparation II (140 g, 0.2282 moles) at 20-25 °C. The reaction mixture was cooled to 0-5 °C and trifluoroacetic acid (980 mL) was charged slowly for 30-40 minutes. The resulting mixture was stirred for 2 hr at 0-5 °C under nitrogen atmosphere. The reaction temperature was raised to 20 to 25 °C, and the reaction mixture was stirred for 1-2 hr at 20 to 25 °C. After completion of the reaction, the reaction mixture was concentrated to dryness at 50 to 55 °C under vacuum. Toluene (3×700 mL,) was charged into the concentrated reaction mass, and then distilled off at 50 to 55 °C under vacuum. After complete concentration from toluene, ethyl acetate (280 mL) was charged into the reaction mass at 20 to 25 °C, stirred for 60 minutes, then the solid was collected by filtration, washed with ethyl acetate (140 mL), dried under vacuum at 50 to 55 °C for 12 hr until loss on drying was less than 2.0%. Obtained Preparation IK (106 g, 84%): HPLC purity: 98.43%.
Example 1 :
[00245] A reaction vessel was charged with Preparation IK (30 g, 53.81 mmol), HOBt (8.7g, 64.38 mmol), and THF (150 mL) at room temperature. To the homogeneous solution was added EDCI (12.4g, 64.68 mmol), stirred for 15 min, then cooled to 8 °C. To the reaction mixture was added ammonia (2M in IP A) (81 mL, 162 mmol) over 5 min so as to maintain a temperature below 10 °C. The resulting heavy slurry was stirred for 10 min, warmed to room temperature over 30 min, then stirred for 4 hr. At the completion of the reaction, water (230 mL) was slowly added over 15 min to maintain a temperature below 20 °C, and then stirred for 2 hr. The solid was collected by filtration, washed with water (3X60 mL), then dried under vacuum 48 hr at 55 °C. The above crude product was charged into a 1 L 3 -necked round flask. IP A (200 mL) was added, then heated to 80 °C resulting in a homogeneous solution. Water (170 mL) was slowly added (15 min) to maintain an internal temperature >75 °C. The resulting slurry was stirred and cooled to room temperature for 2 hr. The solid was collected by filtration, washed with water (2 X 50 mL), then dried under vacuum (55 °C for 24 h, and 30 °C for 48 h).
Obtained Example 1 (23.4 g, 78% yield): HPLC purity: 99.43%.
Example 2 NOT SAME
WITHOUT METHYL GROUP
(2R,35)-N-((35)-2-Oxo-5-phenyl-2,3-dihydro-lH-l,4-benzodiazepin-3-yl)-2,3-bis(3,3,3- trifluoropropyl)succinamide
Preparation 2A: (35)-3-Amino-5-phenyl-l,3-dihydro-2H-l,4-benzodiazepin-2-one, and Preparation 2B: -3-Amino-5-phenyl-l,3-dihydro-2H-l,4-benzodiazepin-2-one
(2A) (2B)
[00246] Racemic 3-amino-5-phenyl-l,3-dihydro-2H-l,4-benzodiazepin-2-one (J. Med. Chem., 49:231 1-2319 (2006), compound# 5) was prepared according to the literature procedure. The enantiomers were separated on Berger SFC MGIII Column: Lux 25X3 cm, 5cm; Mobile phase: 30% MeOH+ 0.1% DEA in C02; Flow rate: 150 mL/min;
Temperature: 40 °C; Detector wavelength: 250 nM. Obtained the S-enantiomer
Preparation 2A as a white solid: XH NMR (400 MHz, DMSO-d6) δ ppm 10.67 (1 H, br. s.), 7.58 (1 H, td, J=7.65, 1.76 Hz), 7.37-7.53 (5 H, m), 7.23-7.30 (2 H, m), 7.14-7.22 (1 H, m), 4.23 (1 H, s), 2.60 (2 H, br. s.); HPLC: RT=3.0625 min (30% MeOH + 0.1% DEA in C02 on OD-H Column, 3 mL/min, 35 °C, 96 bar, 230 nm, ΙΟμΙ inj); [a]D = -208.3° (5.05 mg/niL, MeOH). Also obtained the R-enantiomer Preparation 2B as an off white solid: HPLC: RT=3.970 min; [a]D = 182.1° (2.01 mg/mL, MeOH).
Preparation 2C: tert-Butyl (25,,3R)-6,6,6-trifluoro-3-(((35)-2-oxo-5-phenyl-2,3-dihydro- 1 H- 1 ,4-benzodiazepin-3 -yl)carbamoyl)-2-(3 ,3 ,3 -trifluoropropyl)hexanoate, and
Preparation 2D: tert-Butyl (2R,3R)-6,6,6-trifluoro-3-(((35)-2-oxo-5-phenyl-2,3-dihydro- 1 H- -benzodiazepin-3 -yl)carbamoyl)-2-(3 ,3 ,3 -trifluoropropyl)hexanoate
(2C) (2D)
[00247] Preparation 2C was prepared from Preparation 2A (564 mg, 2.244 mmol) and a mixture of Preparation IE and Preparation IF (822 mg, 2.244 mmol) according to the general procedure shown for Preparation II. Obtained Preparation 2C and Preparation 2D (1.31 g, 97%): HPLC: RT=3.443 min (CHROMOLITH® ODS 4.6 x 50 mm (4 min grad) eluting with 10-90% aqueous MeOH over 4 minutes containing 0.% TFA, 4 mL/min, monitoring at 220 nm); MS (ES): m/z= 600.3 [M+H]+.
Preparation 2E: (25′,3R)-6,6,6-Trifluoro-3-(((35)-2-oxo-5-phenyl-2,3-dihydro-lH-l,4- benzodiazepin-3-yl)carbamoyl)-2-(3,3,3-trifluoropropyl)hexanoic acid, and
Preparation 2F: (2R,3R)-6,6,6-Trifluoro-3-(((35)-2-oxo-5-phenyl-2,3-dihydro-lH-l,4- benzodiazepin-3-yl)carbamoyl)-2-(3,3,3-trifluoropropyl)hexanoic acid
(2E) (2F) [00248] A mixture of Preparation 2E and Preparation 2F was prepared from a mixture of Preparation 2C and Preparation 2D (1.3 lg, 2.185 mmol) by the general methods shown for Preparation IK. Obtained a mixture of Preparation 2E and Preparation 2F (1.18 g, 99%): HPLC: RT=2.885 min (CHROMOLITH® ODS 4.6 x 50 mm (4 min grad) eluting with 10-90% aqueous MeOH over 4 minutes containing 0.% TFA, 4 mL/min, monitoring at 220 nm). MS (ES): m/z= 544.2 [M+H]+.
Example 2:
[00249] Example 2 was prepared from a mixture of Preparation 2E and Preparation 2F (354 mg, 0.651 mmol) by the general methods shown for Example 1. After separation of the diastereoisomers, Example 2 was obtained (188 mg, 52%) as a white solid: HPLC: RT=9.063 min (H20/CH3CN with TFA, Sunfire C18 3.5um, 4.6x150mm, 4.6x150mm, gradient = 15 min, wavelength = 220 and 254 nm); MS (ES): m/z= 543 [M+H]+; XH NMR (400 MHz, DMSO-d6) δ ppm 10.87 (1 H, br. s.), 9.50-9.55 (1 H, m), 7.62-7.69 (2 H, m), 7.40-7.57 (5 H, m), 7.29-7.36 (2 H, m), 7.22-7.28 (1 H, m), 7.16 (1 H, br. s.), 5.25 (1 H, d), 3.30-3.32 (1 H, m), 2.75-2.86 (1 H, m), 2.44-2.48 (1 H, m), 2.06-2.34 (3 H, m), 1.51- 1.77 (4 H, m); [a]D = -114.4° (8.04 mg/mL, DMSO).
[00250] Crystal Form M2- 1 was prepared by adding approximately 1 mg of Example 2 to approximately 0.7 mL of MeOH/fluorobenzene solution (3 : 1). Colorless plate-like crystals were obtained after 2 days of solvent evaporation at room temperature.
Clip
For some disease targets, an indirect approach may be best. Or so Ashvinikumar V. Gavai and his colleagues atBristol-Myers Squibbfound in their quest toward a potential cancer drug. Gavai unveiled BMS-906024, which is an experimental—and slightly roundabout—treatment for a number of cancers, including breast, lung, and colon cancers, and leukemia.
Cancers have a tendency to relapse or to become resistant to treatments that once worked. Research at BMS and elsewhere had suggested that a family of proteins called Notch is implicated in that resistance and in cancer progression more generally. Gavai, director of oncology chemistry at BMS in Princeton, N.J., and his team set out to block Notch family signaling.
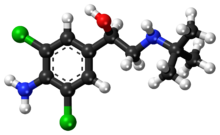
Notch family members lack enzymatic activity, so blocking them directly is difficult. Instead, BMS developed inhibitors of an enzyme that is essential for activating Notch signaling—γ-secretase.
Company: Bristol-Myers Squibb
Disease: breast, lung, colon cancer; leukemia
Interfering with Notch, even in this indirect way, can have detrimental effects on the gastrointestinal tract. Only two of the four Notch family members are linked to that side effect, Gavai says. But he and his team think their drug will be most effective if it acts on all four family members roughly equally—a so-called pan-Notch inhibitor. By selecting a molecule that’s well tolerated in animals and carefully scheduling doses of the drug in humans, it could be possible to minimize side effects, he says.
The BMS team relied on Notch signaling assays in leukemia and breast cancer cell lines to find leads. They soon learned that for their molecules to work, three chiral centers had to be in the S,R,Sconfiguration. After that, they strove to make the molecules last in the bloodstream. They removed an isobutyl group and tweaked some other parts of their candidate’s succinamide side chain. It was tough to retain both a long half-life and activity against Notch, Gavai told C&EN. “You’d optimize one and lose the other.”
His team threaded the needle with BMS-906024. Their studies with mice suggest that a dose of 4–6 mg once a week could be effective in people. That’s lower than doses being tested for other Notch-targeted agents, according to the website clinicaltrials.gov. The mouse studies also back the idea that Notch is involved in cancer drug resistance and suggest that Notch could be a target for taking on cancer stem cells, which are notoriously resistant to chemotherapy.
BMS-906024 is in Phase I clinical trials, both alone and in combination with other agents. Patients with colon, lung, breast, and other cancers are receiving intravenous doses of the compound to determine its safety and optimum dose ranges.
![09116-cover-BMScxd]()
(From left, front row) Gavai, Weifeng Shan, (second row) Aaron Balog, Patrice Gill, Gregory Vite, (third row) Francis Lee, Claude Quesnelle, (rear row) Wen-Ching Han, Richard Westhouse.
Credit: Catherine Stroud Photography
http://cen.acs.org/articles/91/i16/BMS-906024-Notch-Signaling-Inhibitor.html
![Image result for BMS 906024 synthesis]()
clip
![Image result for BMS 906024]()
BMS-906024
Company: Bristol-Myers Squibb
Meant to treat: cancers including breast, lung, colon, and leukemia
Mode of action: pan-Notch inhibitor
Medicinal chemistry tidbit: The BMS team used an oxidative enolate heterocoupling en route to the candidate– a procedure from Phil Baran’s lab at Scripps Research Institute. JACS 130, 11546
Status in the pipeline: Phase I
Relevant documents: WO 2012/129353
PAPER
An enantioselective synthesis of (S)-7-amino-5H,7H-dibenzo[b,d]azepin-6-one (S–1) is described. The key step in the sequence involved crystallization-induced dynamic resolution (CIDR) of compound 7 using Boc-d-phenylalanine as a chiral resolving agent and 3,5-dichlorosalicylaldehyde as a racemization catalyst to afford S–1 in 81% overall yield with 98.5% enantiomeric excess.
† Department of Discovery Synthesis, Biocon Bristol-Myers Squibb Research Centre, Biocon Park, Bommasandra IV Phase, Jigani Link Road, Bengaluru 560099, India
‡Bristol-Myers Squibb Company, P.O Box 4000, Princeton, New Jersey 08543-4000, United States
Org. Process Res. Dev., Article ASAP
1. Quesnelle, Claude; Kim, Soong-Hoon; Lee, Francis; Gavai, Ashvinikumar. Bis(fluoroalkyl)-1,4-benzodiazepinone compounds as Notch receptor inhibitors and their preparation and use in the treatment of cancer. PCT Int. Appl. (2012), WO 2012129353 A1 20120927.
BMS-906024
![BMS-906024.svg]() |
| Systematic (IUPAC) name |
|
(2R,3S)-N-[(3S)-1-Methyl-2-oxo-5-phenyl-2,3-dihydro-1H-1,4-benzodiazepin-3-yl]-2,3-bis(3,3,3-trifluoropropyl)succinamide
|
| Identifiers |
| PubChem |
CID 66550890 |
| ChemSpider |
28536138 |
| Chemical data |
| Formula |
C26H26F6N4O3 |
| Molar mass |
556.500 g/mol |
-
CN1c2ccccc2C(=N[C@@H](C1=O)NC(=O)[C@H](CCC(F)(F)F)[C@H](CCC(F)(F)F)C(=O)N)c3ccccc3
|
CN1c2ccccc2C(=N[C@@H](C1=O)NC(=O)[C@H](CCC(F)(F)F)[C@H](CCC(F)(F)F)C(=O)N)c3ccccc3
![Image result for γ-Secretase Inhibitors BMS]()
Patent US8377886 – Use of gamma secretase inhibitors and notch …
www.google.com
Figure US08377886-20130219-C00003. gamma secretase inhibitor
![Image result for γ-Secretase Inhibitors BMS]()
RO4929097 | γ-secretase inhibitor – Cellagen Technology
Filed under:
PHASE 1,
PHASE1 Tagged:
1401066-79-2,
3,
5-dichlorosalicylaldehyde,
Alzheimer’s Disease,
Ashvinikumar Gavai,
bms,
Boc-D-phenylalanine,
Bristol-Myers Squibb,
CIDR;dibenzoazepenone,
DKR; Notch inhibitors,
γ-secretase inhibitor,
Notch inhibitor,
PHASE 1,
SAR,
T-acute lymphoblastic leukemia,
triple-negative breast cancer ![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()













 Dr Gautam Sethi
Dr Gautam Sethi

 The presentation will load below
The presentation will load below









































 AKEBIA THERAPEUTICS PRESIDENT & CEO JOHN BUTLER PRESENTING AT THE AMERICAN KIDNEY FUND
AKEBIA THERAPEUTICS PRESIDENT & CEO JOHN BUTLER PRESENTING AT THE AMERICAN KIDNEY FUND














































































































































 The presentation will load below
The presentation will load below


























































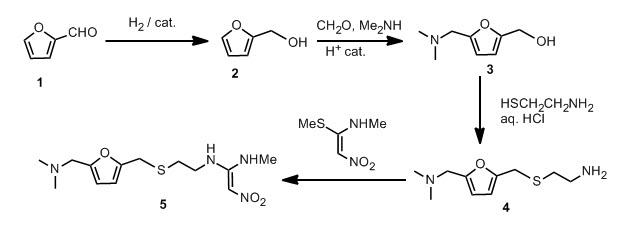
 On with the show, though. The original synthetic route was provided in the paper and I will provide it to you.
On with the show, though. The original synthetic route was provided in the paper and I will provide it to you.




 .
.