
VILDAGLIPTIN
- Molecular FormulaC17H25N3O2
- Average mass303.399 Da
- (2S)-1-{2-[(3-hydroxyadamantan-1-yl)amino]acetyl}pyrrolidine-2-carbonitrile
(2S)-1-[N-(3-Hydroxyadamantan-1-yl)glycyl]pyrrolidine-2-carbonitrile(2S)-1-[N-(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)glycyl]pyrrolidine-2-carbonitrile274901-16-5[RN]2-Pyrrolidinecarbonitrile, 1-[2-[(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)amino]acetyl]-, (2S)-(-)-(2S)-1-[[(3-Hydroxytricyclo[3.3.1.1[3,7]]dec-1-yl)amino]acetyl]pyrrolidine-2-carbonitrile
(2S)-1-[N-(3-Hydroxyadamantan-1-yl)glycyl]-2-pyrrolidinecarbonitrile
Vildagliptin was approved by the European Medicines Agency (EMA) on Sep 26, 2007, and approved by Pharmaceuticals and Medical Devices Agency of Japan (PMDA) on Jan 20, 2010, following by China Food and Drug Administration (CFDA) on Aug 15, 2011. It was developed and marketed as Galvus® by Novartis in EU.
Vildagliptin is a potent selective inhibitor of dipeptidyl peptidase-4 (DPP-4) that improves glycaemic control by increasing islet α-cell and β-cell responsiveness to glucose. It is used to reduce hyperglycemia in type 2 diabete.
Galvus®is available as film-coated tablet for oral use, containing 50 mg free Vildagliptin. The recommended dose of vildagliptin is 100 mg, administered as one dose of 50 mg in the morning and one dose of 50 mg in the evening.Drug Name:VildagliptinResearch Code:LAF-237; DSP-7238; NVP-LAF-237Trade Name:Galvus® / Jalra® / Xiliarx® / Equa®MOA:Dipeptidyl peptidase-4 (DPP-4) inhibitorIndication:Type 2 diabetesStatus:ApprovedCompany:Novartis (Originator)Sales:$1,140 Million (Y2015); 
$1,224 Million (Y2014);
$1,200 Million (Y2013);
$910 Million (Y2012);
$677 Million (Y2011);ATC Code:A10BH02
Approved Countries or AreaUpdate Date:2015-07-29
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2008-11-19 | Marketing approval | Xiliarx | Type 2 diabetes | Tablet | 50 mg | Novartis | |
| 2008-11-19 | Marketing approval | Jalra | Type 2 diabetes | Tablet | 50 mg | Novartis | |
| 2007-09-26 | Marketing approval | Galvus | Type 2 diabetes | Tablet, Film coated | 50 mg | Novartis |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2010-01-20 | Marketing approval | Equa | Type 2 diabetes | Tablet | 50 mg | Novartis |
| Approval Date | Approval Type | Trade Name | Indication | Dosage Form | Strength | Company | Review Classification |
|---|---|---|---|---|---|---|---|
| 2011-08-15 | Marketing approval | 佳维乐/Galvus | Type 2 diabetes | Tablet | 50 mg | Novartis | |
| 2011-08-15 | Marketing approval | 佳维乐/Galvus | Type 2 diabetes | Tablet | 50 mg | Novartis |
Vildagliptin, previously identified as LAF237, is a new oral anti-hyperglycemic agent (anti-diabetic drug) of the new dipeptidyl peptidase-4 (DPP-4) inhibitor class of drugs. Vidagliptin subsequently acts by inhibiting the inactivation of glucagon-like peptide-1 (GLP-1) and gastric inhibitory polypeptide (GIP) by DPP-4. This inhibitory activity ultimately results in a two-fold action where GLP-1 and GIP are present to potentiate the secretion of insulin by beta cells and suppress glucagon secretion by alpha cells in the islets of Langerhans in the pancreas. It is currently in clinical trials in the U.S. and has been shown to reduce hyperglycemia in type 2 diabetes mellitus. While the drug is still not approved for use in the US, it was approved in Feb 2008 by European Medicines Agency for use within the EU and is listed on the Australian PBS with certain restrictions.
Vildagliptin, sold under the brand name Galvus among others, is an oral anti-hyperglycemic agent (anti-diabetic drug) of the dipeptidyl peptidase-4 (DPP-4) inhibitor class of drugs. Vildagliptin inhibits the inactivation of GLP-1[2][3] and GIP[3] by DPP-4, allowing GLP-1 and GIP to potentiate the secretion of insulin in the beta cells and suppress glucagon release by the alpha cells of the islets of Langerhans in the pancreas.
Vildagliptin has been shown to reduce hyperglycemia in type 2 diabetes mellitus.[2]
Combination with metformin
The European Medicines Agency has also approved a combination of vildagliptin and metformin, vildagliptin/metformin (Eucreas by Novartis) as an oral treatment for type-2 diabetes.[4]
Adverse effects
Adverse effects observed in clinical trials include nausea, hypoglycemia, tremor, headache and dizziness. Rare cases of hepatoxicity have been reported.[5]
There have been case reports of pancreatitis associated with DPP-4 inhibitors. A group at UCLA reported increased pre-cancerous pancreatic changes in rats and in human organ donors who had been treated with DPP-4 inhibitors.[6][7] In response to these reports, the United States FDA and the European Medicines Agency each undertook independent reviews of all clinical and preclinical data related to the possible association of DPP-4 inhibitors with pancreatic cancer. In a joint letter to the New England Journal of Medicines, the agencies stated that “Both agencies agree that assertions concerning a causal association between incretin-based drugs and pancreatitis or pancreatic cancer, as expressed recently in the scientific literature and in the media, are inconsistent with the current data. The FDA and the EMA have not reached a final conclusion at this time regarding such a causal relationship. Although the totality of the data that have been reviewed provides reassurance, pancreatitis will continue to be considered a risk associated with these drugs until more data are available; both agencies continue to investigate this safety signal.”[8]
PATENT
https://patents.google.com/patent/US20080167479A1/en
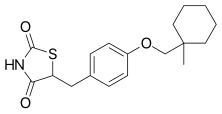
- Vildagliptin is an active pharmaceutical substance with an empirical formula of C17H25N3O2 and a molecular weight of 303.40 g/mol. Vildagliptin is the international common accepted name for (2S)-1-[[(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)amino]acetyl]-2-pyrrolidine carbonitrile and has the structure of formula (I).
- [0003]Vildagliptin is a dipeptidyl peptidase IV (DPP-IV) inhibitor and is disclosed in U.S. Pat. No. 6,166,063 (“the ‘063 patent”), the disclosure of which is incorporated herein by reference. The ‘063 patent discloses a synthesis of vildagliptin using the synthetic process represented in Scheme 1.
- [0004]Vildagliptin can exist as the (2S) and (2R) enantiomers. The stereoisomer with the desired biological activity is the (2S) enantiomer. Accordingly, it is desirable to synthesize (2S)-vildagliptin with high stereochemical purity. A process that yields vildagliptin with a high enantiomeric purity is disclosed in International Patent Publication WO 2004/092127, the disclosure of which is incorporated herein by reference. This reference discloses compositions containing from 95% to 99.99% of (2S)-vildagliptin.
- [0069]This example illustrates the synthesis of the compound of formula (I) in accordance with embodiments of the invention.
- [0070]Into a 100 mL rounded reaction vessel were charged 3 g (17.37 mmol) of 1-chloroacetyl-2-cyanopyrrolidine, 3.22 g (19.82 mmol) of 1-amino-3-adamantanol, 2.78 g (20.1 mmol) of potassium carbonate, and 30 mL isopropyl acetate. The mixture was refluxed for 4 h, cooled to room temperature, and the salts were filtered and washed with acetonitrile. The mother liquors were evaporated to dryness to obtain an oil which was aged in MEK from which a white solid crystallizes at 0-5° C. The solid was filtered washing the cake with MEK and dried at 40° C. in a vacuum oven until constant weight.
- [0071]Yield: 36%. Assay: 99.21%. HPLC purity: 97.55% of vildagliptin (measured according to Example 2). HPLC chiral purity: more than 99.99% of vildagliptin (measured according to Example 7).
- [0072]These results demonstrate that a compound of formula (I) comprising less than 0.01% of (2R)-1-[N-(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)glycyl]-2-pyrrolidinecarbonitrile (i.e., (2R)-vildagliptin).
Patent
https://patents.google.com/patent/WO2015145467A1/en
Vildagliptin is chemically known as (S)-l-[2-(3-Hydroxyadamantan-l-ylamino) acetyl] pyrrolidine-2-carbonitrile and exist as (2S) and (2R) enantiomers. The stereoisomer with the desired biological activity is the (2S) enantiomer, represented by the following structure:

U.S. Patent No. 6,166,063 (“the Ό63 patent”) discloses new class of Dipeptidyl peptidase 4 (DPP-4) inhibitors such as vildagliptin. The ‘063 patent further discloses a process for the preparation of vildagliptin by acylation of L-prolinamide with chloroacetyl chloride in the presence of a base in dichloromethane or tetrahydrofuran as solvent, filtration and subsequent dehydration with trifluoroacetic anhydride (TFAA) to provide (S) -1- (2- chloroacetyl) pyrrolidin-2-carbonitrile. The carbonitrile intermediate is isolated by distilling out the solvent, co-distillation with ethyl acetate, partitioning between water and ethyl acetate, extraction of the resulting aqueous layer with ethyl acetate followed by aqueous washings of the organic layer and concentrating to obtain carbonitrile intermediate as yellow solid. This is later reacted with about 2 moles of l-aminoadamantane-3-ol in the presence of about 4 moles of potassium carbonate in dichloromethane (DCM) or tetrahydrofuran (THF) for 6 days. Finally, the obtained crude vildagliptin is subjected to chromatography employing SIMS/Biotage Flash chromatography system providing vildagliptin with melting point of 138°C-140°C. The disclosed process is schematically represented as follows:

Amide Carbonitrile
A similar process is described in J. Med. Chem. 2003, 46, 2774-2789, where acylation of L-prolinamide with chloroacetyl chloride is carried out in the presence of potassium carbonate in tetrahydrofuran as solvent and subsequent dehydration with TFAA to provide (S) -1- (2-chloroacetyl) pyrrolidin-2 -carbonitrile. The carbonitrile intermediate was isolated by adding ethyl acetate, distillation of the solvent, partitioning between water and aqueous sodium bicarbonate, extraction of the resulting aqueous layer with ethyl acetate followed by aqueous washings of the organic layer and concentrating to obtain carbonitrile intermediate as yellow- white solid which was reacted with about 2-3 moles of 1- aminoadamantane-3-ol in the presence of about 3 moles of potassium carbonate in DCM or THF for 1-3 days followed by purification from a mixture of ethyl acetate and isopropanol provided Vildagliptin as a white solid.
U.S. Patent No. 6,011,155 discloses a process for the preparation of (S) -1- (2- bromooacetyl) pyrrolidin-2-carbonitrile by acylation of L-prolinamide with bromoacetyl bromide in the presence of triethyl amine and catalytic amount of DMAP in DCM as solvent wherein the resulting (S)-l -(2 -bromoacetyl) pyrrolidin-2-carboxamide is isolated and subsequently dehydrated with TFAA to obtain the carbonitrile intermediate as dark yellow solid.
U.S. Patent application No. 2008/0167479 discloses preparation of Vildagliptin with high chemical and enantiomeric purities wherein (S) -1- (2-chloroacetyl) pyrrolidin-2- carbonitrile is prepared in one step process by acylation of prolinamide with chloroacetyl chloride in a mixture of isopropyl acetate and DMF followed by dehydration with cyanuric chloride to obtain the carbonitrile intermediate as an oil which was crystallized from isopropanol. The resulting carbonitrile intermediate is reacted with l-aminoadamantane-3- ol in the presence of alkali metal carbonates such as potassium carbonate and an optional additive such as I in a solvent comprising at least an ester or ether or nitrile solvent and purification of vildagliptin from methyl ethyl ketone or from a mixture of isopropanol and methyl t-butyl ether.
PCT Publication No. 2010/022690 discloses a process for the preparation of vildagliptin wherein (S)-l -(2-chloroacetyl) pyrrolidin-2-carboxamide intermediate is isolated as a trialkylamine hydrohalide salt in two fractions and. dehydrated with TFAA to obtain (S)-l- (2-chloroacetyl) pyrrolidin-2-carbonitrile as light yellow powder after crystallization from heptane. The resulting carbonitrile intermediate is then reacted with 3-amino-l- adamantanol in the presence of alkali metal carbonate base and an alkali metal iodide as a catalyst in a mixture of organic ketones, ester and polar aprotic solvents. The crude product was subjected to multiple crystallizations in order to achieve high chemical purity of vildagliptin. This publication also disclosed final crystallization of vildagliptin from 2- butanone, toluene, 2-methyl tetrahydrofuran, isopropyl acetate, dimethyl carbonate, isopropanol. This process adds an extra step of isolation of the said carboxamide intermediate, uses mixture of solvents in the preparation of vildagliptin and to multiple crystallizations which makes the process uneconomical on large scale.
PCT Publication No. 2011/101861 discloses a process for the preparation of vildagliptin wherein (S)-l-(2-chloroacetyl) pyrrolidin-2-carboxamide and (S)-l-(2-chloroacetyl) pyrrolidin-2-carbonitrile intermediates are isolated as solids after purification and drying. Further, (S)-l-(2-chloroacetyl) pyrrolidin-2-carbonitrile is then converted to vildagliptin by reacting it with l-aminoadamantane-3-ol in the presence of potassium carbonate and KI in a suitable ether solvent like THF and purifying the obtained vildagliptin from a mixture of ethyl acetate and methanol. This publication also provided an alternate process for the preparation of vildagliptin by reacting 2-(3-hydroxyadamantan-l-yl amino) acid or derivative thereof with pyrrolidine-2-carbonitrile and various solvents from which vildagliptin may be crystallized such as ethyl acetate, 2-butanone, or mixture of ethyl acetate-methanol, ethyl acetate-isopropanol, methanol-DCM, ethyl acetate-cyclohexane and 2-butanone-methyl t-butyl ether.
U.S. Patent No. 7,375,238 discloses a one-pot process for the preparation of vildagliptin without isolation of the carboxamide and carbonitrile intermediates and further involves preparation of Vildagliptin by using potassium carbonate and potassium iodide (KI) as catalysts in 2-butanone solvent. Purification of the crude vildagliptin was carried out from a mixture of isopropanol and methyl t-butyl ether in the presence of 1,8- diazabicyclo[5.4.0]undec-7-ene (DBU) base and final recrystallization from 2-butanone afforded pure vildagliptin. This process suffers from certain draw backs such as use of mixture of solvents for the acylation and condensation reactions; use of base and expensive additive such as KI in the condensation reaction.
PCT Publication No. 2011/012322 discloses a process wherein the (S) -1- (2-chloroacetyl) pyrrolidin-2-carbonitrile intermediate is isolated, purified and reacted with 1- aminoadamantane-3-ol in the presence of a phase transfer catalyst, optionally an inorganic base and a solvent selected from nitrile, ketone, ether, ester and mixtures thereof in a two phase reaction system wherein the first phase consist of a liquid phase and the second phase consists of an inorganic base. The final purification of vildagliptin was carried out in 2- butanone solvent.
PCT Publication No. 2013/179300 discloses preparation of vildagliptin from organic solvents such as aromatic hydrocarbons, aliphatic hydrocarbons, halogenated hydrocarbons, ethers, nitrile, dialkyl formamides, dialkylacetamides, dialkyl sulfoxides in the presence of organic or inorganic base. The resulting crude vildagliptin was purified by acid-base treatment and crystallization from a solvent selected from aliphatic hydrocarbons, aromatic hydrocarbons, ketones, esters, nitrile, ether, cyclic ether and alcohol or mixtures thereof.
PCT Publication No. 2012/022994 involves conversion of racemic vildagliptin to (S)- enantiomer via formation of vildagliptin adducts and final purification from ethyl acetate or mixture of ethyl acetate with 1% water.
U.S. Application No. 2006/0210627 discloses crystalline Form A of vildagliptin and its preparation from 2-butanone, isopropanol, acetone or a mixture of isopropanol-ethyl acetate in the presence of DBU base. This publication also discloses amorphous vildagliptin and its preparation by lyophilization from a water solution.
PCT Publication No. 2014/102815 disclosed a process for the preparation of vildagliptin by isolating the carboxamide and carbonitrile intermediates after crystallization and drying. The resulting carbonitrile intermediate is reacted with l-aminoadamantane-3-ol in the presence of organic base or inorganic base in nitrile, ester or alcohol solvent.
IN 3965 MUM/2013 publication discloses a process for the preparation of vildagliptin by preparing and crystallizing (S) -1- (2-chloroacetyl) pyrrolidin-2-carbonitrile intermediate and reacting it with l-aminoadamantane-3-ol in the presence of a potassium carbonate, optionally in presence of suitable catalyst such as KI in ketone solvent or in mixture of ketone with non polar solvents.
C.N. publication No. 102617434 discloses a one pot process for the preparation of Vildagliptin by reacting salt of pyrrolidine carbonitrile such as TFA salt with haloacetyl halide in the presence of a base followed by insiru reaction with l-aminoadamantane-3-ol in the presence of tertrabutyl ammonium iodide in halogenated hydrocarbon or ether as solvent to get vildagliptin which is further crystallized from ethyl acetate-petroleum ether.
C.N. publication No. 103804267 discloses a process for the preparation of vildagliptin by reacting (S)-l -(2 -haloacetyl) pyrrolidin-2-carbonitrile with l-aminoadamantane-3-ol in a mixed system of an organic solvent and water in the presence of a base and phase transfer catalyst followed by crystallization of the obtained crude vildagliptin.
C.N. publication No. 103787944 disclosed dehydration of-1- (2-chloroacetyl) -2- (S) – pyrrolidine carboxamide in the presence of a dehydrating agent and an acid-binding agent in an organic solvent followed by crystallization from mixture of isopropyl ether and ethyl acetate to provide l-(2-chloroacetyl)-2-(S)-pyrrolidine carbonitrile as white or pale yellow solid powder.
Furthermore, several techniques are known in the art for the purification of vildagliptin such as chromatography (US 6,166,063); or acid-base purification (IN 61 /MUM/2012 publication) or via formation of inorganic salt complexes (WO 2011/042765); or by solvent crystallizations such as mixture of ethyl acetate and isopropanol (J. Med. Chem. 2003, 46, 2774-2789); isopropanol and MTBE in the presence of DBU base and final recrystallization from 2-butanone (US 7,375,238); methyl ethyl ketone or from a mixture of isopropanol and MTBE (US 2008/0167479); acetone, 2-butanone, cyclohexanone, ethyl acetate, isopropyl acetate or dimethyl carbonate (IN 61 /MUM/2012 publication); 2- butanone (WO 2011/012322); aliphatic hydrocarbons, aromatic hydrocarbons, ketones, esters, nitrile, ether, cyclic ether and alcohol or mixtures thereof (WO 2013/179300); or from ethyl acetate or mixture of ethyl acetate with 1% water (WO 2012/022994).
Most of the processes known in the art for synthesizing vildagliptin are associated with one or more of the following disadvantages:
a) use of toxic TFAA for dehydration which is costly and environmentally harmful, b) lengthy and time consuming condensation process,
c) conventional solvents used in the condensation stage are costly, volatile, flammable, toxic, causing adverse health effects, in, addition to this potentially unsafe peroxide forming solvents such as THF were used, which process is more costlier than the process not having such elements,
d) purification of vildagliptin by chromatographic purification or by formation of inorganic salt complexes or by multiple crystallizations which are tedious, labor intensive, uses high amounts of solvents, require precise monitoring and time consuming and hence not viable for commercial scale operations.
Therefore, the present invention fulfills the need in the art and provides simple, industrially feasible and scalable processes for the preparation and purification of vildagliptin that circumvent disadvantages associated with the prior art process, proved to be advantageous from environmental and industrial point of view and also fulfill purity criteria. These processes allow the final product to be produced in a higher yield and purity by minimizing number of processing steps and reducing the number of solvent usage which is very practical for scale-up production, especially in terms of operating efficiency.
The new processes has a further advantage in recovering the expensive 1- aminoadamantane-3-ol from the reaction mixture and recycling in a simple manner that avoids use of inorganic salt complexes, which is economical and applicable on an industrial scale.
EXAMPLE 1: Preparation of (2S)- 1 -(Chloroacetyl)-2-pyrrolidinecarbonitrile.
To a solution of L-Prolinamide (100 gms) dissolved in DCM (1000 mL) was added triethyl amine (88.6 gms) and DMAP (1.07 gms) at 25-30°C under N2 atmosphere and stirred for 15 min at 25-30°C. This solution was added to a solution of chloroacetyl chloride (98.9 gms) in DCM (500 mL) under N2 atmosphere at -5 to 0°C over 2-3 hr. Raised the reaction mass temperature to 0-5°C and stirred for lhr. After reaction completion, charged phosphorus oxy chloride (201.5 gms) to the reaction mass at 0-5 °C, heated the reaction mass temperature to reflux and stirred for 6hr at same temperature. After reaction completion, allowed to cool to 10-20°C and added DM water (500 mL). Aqueous layer was separated and the organic layer was washed with DM water. To the organic layer DM water (300 mL) was added at 25-30°C and adjusted the reaction mass pH to 6.5-7.5 with -500 mL of sodium bicarbonate solution (-40 g of NaHC03 dissolved in 500 mL of DM Water). Separated the aqueous layer and concentrated the organic layer under vacuum at temperature of 30-40°C to get residual mass. Charged isopropanol (100 mL) and distilled out solvent completely under vacuum at <50°C. The resulting residue was allowed to cool to 30-40°C and charged isopropanol (500 mL). Heated the reaction mass temperature to 40- 45°C, stirred for 30 min at 40-45°C, allowed to cool to 0-5°C, stirred for 2 hr, filtered and washed wet cake with chilled isopropanol (100 mL), dried at 40-45°C for 6 hr to provide 115 gms of (2S)-l-(CMoroace1yl)-2-pyrrolidinecarbonitrile.
HPLC Purity: 99.86%.
Example 2: Preparation of Vildagliptin
To (2S)-l-(Chloroacetyl)-2 -Pyrrolidine carbonitrile (100 gms) dissolved in DM Water (500 mL), charged l-aminoadamantane-3-ol (242.2 g) at 25-35°C. Heated the reaction mass temperature to 40-45°C and stirred for 8-10 hr at 40-45°C. After reaction completion, allowed to cool to 25-30°C and charged DM water (700 mL) and DCM (600 mL). Separated the organic layer and extracted the aqueous layer with DCM. The total organic layer was concentrated under vacuum at temperature 30-40°C to get residual mass. Ethyl acetate (100 mL) was added to the residual mass and distilled completely under vacuum at <50°C. Charged ethyl acetate (500 mL) and refluxed for 1 hr. Allowed to cool to 25-30°C and stirred for 2 hr. Filtered the reaction mass and washed with ethyl acetate (100 mL) then dried at 50-55°C for 6 hr to provide 130 gms of crude vildagliptin.
HPLC Purity: 99.56%.
Dimer impurity content: <0.32%;
R-isomer content (by chiral HPLC): <0.2%;
l-aminoadamantane-3-ol content (by GC): 0.56%.
EXAMPLE 3: Preparation of Vildagliptin (using K2C03 and KI)
To l-aminoadamantane-3-ol (19.4 g) taken in DM Water (50 mL), added potassium carbonate (8.0 gms), potassium iodide (0.1 gm) and stirred for 15 mins at 25-35°C. (2S)-1- (Chloroacetyl)-2-Pyrrolidine carbonitrile (10 gms) was added at 25-35°C and stirred for 15 mins at 25-35°C. Raised the reaction mass temperature to 40-45°C and stirred for 4 hr at 40-45°C. After reaction completion, cooled to 25-30°C and charged DCM (50 mL). Separated the organic layer and extracted the aqueous layer with DCM. The total organic layer was washed with DM water and the resulting organic layer was concentrated under vacuum at temperature <40°C to get residual mass. Charged ethyl acetate (70 mL) to above residual mass and refluxed for 1 hr. Cooled to 25-30°C and stirred for 2 hr. Filtered the reaction mass and wash wet cake with ethyl acetate (10 mL). Suck dried for 30 min, dried initially at 25-35°C for 1 hr and then at 50-55°C for 6 hr to provide 12 gms of crude vildagliptin.
HPLC Purity: 99.11%
Dimer impurity content: 0.50%; R-isomer content (by chiral HPLC): not detected
1- aminoadamantane-3-ol content (by GC): 2.09%.
EXAMPLE 4; Preparation of Vildagliptin (using K2HP04 buffer and KI)
·
To l-aminoadamantane-3-ol (19.4 g) taken in DM Water (100 mL), added K2HP04 (10.1 gms), potassium iodide (0.1 gm) and stirred for 15 rnins at 25-35°C. (2S)-l-(Chloroacetyl)-
2- Pyrrolidine carbonitrile (10 gms) was added at 25-35°C and stirred for 15 mins at 25- 35°C. Raised the reaction mass temperature to 40-45°C and stirred for 8-10 hr at 40-45°C. After reaction completion, cooled to 25-30°C and filtered the reaction mass to remove salts. The resulting filtrate was extracted with DCM, and the resulting organic layer was concentrated initially by atmospheric distillation and later under vacuum at temperature 30- 40°C to get residual mass. Charged ethyl acetate (50 mL) to above residual mass and refluxed for 1 hr. Cooled to 25-30°C and stirred for 2 hr. Filtered the reaction mass and washed the wet cake with ethyl acetate (10 mL). Suck dried for 30 min, dried initially at 25-35°C for 1 hr and then at 50-55°C for 6 hr to provide 12 gms of crude vildagliptin.
HPLC Purity: 96.54%
Dimer impurity content: 2.55%;
R-isomer content (by chiral HPLC): not detected
l-aminoadamantane-3-ol content (by GC): 0.86%.
Example 5: Purification of Vildagliptin.
Vildagliptin crude (100 gms) was dissolved in isopropanol (900 mL) by heating to 50-55°C and stirred for 30 min. Filtered the reaction mass over hyflo bed (10 gms) at 50-55°C and washed the hyflo bed with hot isopropanol (100 mL). Distilled out solvent under vacuum at
35-40°C up to 4 volumes remains and allowed to cool to 20-25°C and stirred for 1 hr at same temperature. Further, allowed to cool to 5-10°C, stirred for 2 hrs, filtered and washed with isopropanol (100 mL). The wet product was dried at 50-55°C under vacuum for 8 hr to provide 80 gms of pure vildagliptin.
HPLC Purity: 99.89%;
Dimer impurity content: <0.1 %;
R-isomer content (by chiral HPLC): not detected
l-aminoadarnantane-3-ol content (by GC): 0.06%.
The purified vildagliptin (I) was analyzed by powder X-ray diffraction (PXRD) and is set forth in Figure. 01.
EXAMPLE 6: Preparation of Vildagliptin To a solution of L-Prolinamide (100 gms) dissolved in DCM (1000 mL) was added triethyl amine (88.6 gms) and DMAP (1.07 gms) at 25-30°C under N2 atmosphere and stirred for 15 min at 25-30°C. This solution was added to a solution of chloroacetyl chloride (118.7 gms) in DCM (500 mL) under N2 atmosphere at -5 to 0°C over 2-4 hr. Heated the reaction mass temperature to 10-15°C and stirred until reaction completion, charged phosphorus oxychloride (201.5 gms) to the reaction mass at 0-5°C, heated the reaction mass temperature to reflux and stirred for 6hr at same temperature. After reaction completion, allowed to cool to 5-15°C and slowly added DM water (500 mL). Aqueous layer was separated and the organic layer was washed with DM water. To the organic layer, DM water (300 mL) was added at 25-30°C and adjusted the reaction mass pH to 6.5-7.5 with -200 mL of sodium bicarbonate solution (-16 g of NaHC03 dissolved in 200 mL of DM Water). Separated the aqueous layer and concentrated the organic layer under vacuum at temperature of 30-40°C to get residual mass. The residual mass was dissolved in DM Water (640 mL), charged l-aminoadamantane-3-ol (310.6 g) at 25-35°C. Heated the reaction mass temperature to 40-45 °C and stirred for 9 hr at the same temperature. After reaction completion, allowed to cool to 25-30°C and charged DM water (900 mL) and DCM (1280 mL). Separated the organic layer and extracted the aqueous layer with DCM. The aqueous layer was separated and kept aside for l-aminoadamantane-3-ol recovery. The total organic layer was treated with P.S. 133 carbon, stirred for 30 rnins at 25-30°C and filtered over hyflo bed. The resulting filtrate was concentrated under, vacuum at temperature 30-40°C to get residual mass. To the residual mass, charged ethyl acetate (128 mL) and distilled completely under vacuum at 30-40°C to get semi solid mass. Charged ethyl acetate (640 mL) to the obtained semi solid and refluxed for 1 hr. The reaction mass was allowed to cool to 25-30°C and stirred for 2 hr. Filtered the reaction mass and washed with ethyl acetate (128 mL) to obtain wet cake. Again charged ethyl acetate (512 mL) to the obtained wet cake and refluxed for 1 hr. The reaction mass was allowed to cool to 25- 30°C and stirred for 2 hr. Filtered the reaction mass and washed with ethyl acetate (128 mL) and then dried at 50-55°C for 6 hr to provide 175 gms of crude vildagliptin.
HPLC Purity: 99.66%.
Dimer impurity content: <0.2%;
R-isomer content (by chiral HPLC) : <0.1 %;
l-aminoadamantane-3-ol content (by GC): <0.7%.
DSC: 150.12°C.
EXAMPLE 7: Purification of Vildagliptin. Vildagliptin crude (100 gms) was dissolved in isopropanol (1100 mL) by heating to 50- 55°C and stirred for 30 min. Filtered the solution over hyflo bed at 50-55°C and wash with hot isopropanol (100 mL). Distilled out solvent under vacuum at <55°C up to 5 volumes remains and allowed to cool to 20-25 °C and stirred for 1 hr at same temperature. Further allowed to cool to 10-15 °C, stirred for 2 hrs, filtered and washed with chilled isopropanol (100 mL). The wet product was dried at 50-55°C under vacuum for 8 hr to provide 80 gms of pure vildagliptin. HPLC Purity: >99.8%;
Dimer impurity content: <0.1%;
R-isomeri content (by chir‘al HPLC) : <0.1%;
l-aminoadamantane-3-ol content (by GC): <0.1%.
DSC: 151.92°C.
Example 8: Recovery of l-aminoadamantane-3-ol of formula (IV).
To aqueous layer (1700 mL) from example 1, 50% C.S.lye (435 mL) was added to adjust the pH to 13.0-14.0 at 25-35°C and stirred for 15 mins at 25-35°C. Raised the reaction mass temperature to 60-70°C and stirred for 3 hrs. Cooled to 25-35°C and added DCM (1700 mL), stirred for 15 min and separated the organic layer. The aqueous layer was extracted with DCM and the total organic layer was distilled out completely under vacuum at <40°C to get semisolid mass. Charged ethyl acetate (150 mL) and distilled out solvent completely under vacuum at <50°C to get semisolid material. Charged ethyl acetate (400 mL), stirred for 30 min at 40-45°C and cooled to 25-35°C. Further allowed to cool to 0- 5°C, stirred for 2hr, filtered the reaction mass at 5-10°C and washed with ethyl acetate (100 mL). The wet product was dried at 50-55°C under vacuum for 8 hr to obtain 140 gms of 1- aminoadamantane-3-ol.
Purity by GC: 99.8 %.PATENTS AND PAPERS
Reference:1. WO2004092127A1.
2. WO0034241A1.
3. J. Med. Chem. 2003, 46, 2774-2789.
4. WO2010022690A2.
5. WO2011012322A2.
6. WO2011101861A1.

Reference:1. Beilstein J. Org. Chem. 2008, 4, 20.

Reference:1. WO2011101861A1.
Reference:1. WO2011101861A1.

Reference:1. WO2011101861A1.

Reference:1. WO2012004210A1.




SYN

PAPER
https://www.sciencedirect.com/science/article/abs/pii/S0040403917309176
An original synthesis of vildagliptin ((S)-1-[2-(3-hydroxyadamantan-1-ylamino)acetyl]pyrrolidine-2-carbonitrile), a powerful DPP-4 inhibitor, was developed. Vildagliptin was assembled from 3-amino-1-adamantanol, glyoxylic acid and l-prolinamide in a 4-step reaction sequence with the isolation of only two intermediates. The procedure is competitive with existing protocols, leading to vildagliptin in 63% overall yield.



PAPER
A Facile and Economical Method to Synthesize Vildagliptin
Author(s): Yu Deng, Anmin Wang, Zhu Tao, Yingjie Chen, Xinmei Pan, Xiangnan Hu
Journal Name: Letters in Organic Chemistry
Volume 11 , Issue 10 , 2014
DOI : 10.2174/1570178611666140922121805

A mild and economical method to prepare vildagliptin had been reported with a good yield. In this paper, vildagliptin was synthesized from L-proline and 3-amino-1-adamantanol through chloride acetylation, amination, dehydration and substitution. The total yield of the target compound was 59%.
References
- ^ WHO International Working Group for Drug Statistics Methodology (August 27, 2008). “ATC/DDD Classification (FINAL): New ATC 5th level codes”. WHO Collaborating Centre for Drug Statistics Methodology. Archived from the original on May 6, 2008. Retrieved September 5, 2008.
- ^ Jump up to:a b Ahrén, B; Landin-Olsson, M; Jansson, PA; Svensson, M; Holmes, D; Schweizer, A (2004). “Inhibition of dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels, and reduces glucagon levels in type 2 diabetes”. The Journal of Clinical Endocrinology and Metabolism. 89 (5): 2078–84. doi:10.1210/jc.2003-031907. PMID 15126524.
- ^ Jump up to:a b Mentlein, R; Gallwitz, B; Schmidt, WE (1993). “Dipeptidyl-peptidase IV hydrolyses gastric inhibitory polypeptide, glucagon-like peptide-1(7-36)amide, peptide histidine methionine and is responsible for their degradation in human serum”. European Journal of Biochemistry / FEBS. 214 (3): 829–35. doi:10.1111/j.1432-1033.1993.tb17986.x. PMID 8100523.
- ^ “EU approves Novartis’s Eucreas diabetes drug”. Reuters. February 25, 2008.
- ^ “Galvus” (PDF). http://www.ema.europa.eu. Retrieved July 29, 2018.
- ^ Matveyenko AV, Dry S, Cox HI, et al. (July 2009). “Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin”. Diabetes. 58 (7): 1604–15. doi:10.2337/db09-0058. PMC 2699878. PMID 19403868.
- ^ Butler AE, Campbell-Thompson M, Gurlo T, Dawson DW, Atkinson M, Butler PC (July 2013). “Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors”. Diabetes. 62 (7): 2595–604. doi:10.2337/db12-1686. PMC 3712065. PMID 23524641.
- ^ Egan, Amy G.; Blind, Eberhard; Dunder, Kristina; De Graeff, Pieter A.; Hummer, B. Timothy; Bourcier, Todd; Rosebraugh, Curtis (2014). “Pancreatic Safety of Incretin-Based Drugs — FDA and EMA Assessment — NEJM” (PDF). New England Journal of Medicine. 370 (9): 794–7. doi:10.1056/NEJMp1314078. PMID 24571751.
External links
- “Vildagliptin”. Drug Information Portal. U.S. National Library of Medicine.
- Banting and Best Diabetes Centre at UT vildagliptin – Vildagliptin
- Banting and Best Diabetes Centre at UT dpp4 – About DPP-4
- The race to get DPP-4 inhibitors to market – Forbes.com
- Merck’s March Madness – Forbes.com
| Clinical data | |
|---|---|
| Trade names | Galvus, Xiliarx, Jalra, others |
| Other names | LAF237 |
| AHFS/Drugs.com | UK Drug Information |
| License data | EU EMA: by INN |
| Pregnancy category | Not recommended |
| Routes of administration | By mouth |
| ATC code | A10BH02 (WHO) A10BD08 (WHO) (with metformin)[1] |
| Legal status | |
| Legal status | UK: POM (Prescription only)EU: Rx-onlyIn general: ℞ (Prescription only) |
| Pharmacokinetic data | |
| Bioavailability | 85% |
| Protein binding | 9.3% |
| Metabolism | Mainly hydrolysis to inactive metabolite; CYP450 not appreciably involved |
| Elimination half-life | 2 to 3 hours |
| Excretion | Kidney |
| Identifiers | |
| IUPAC name[show] | |
| CAS Number | 274901-16-5 |
| PubChem CID | 6918537 |
| IUPHAR/BPS | 6310 |
| DrugBank | DB04876 |
| ChemSpider | 5293734 |
| UNII | I6B4B2U96P |
| KEGG | D07080 |
| ChEMBL | ChEMBL142703 |
| CompTox Dashboard (EPA) | DTXSID80881091 |
| ECHA InfoCard | 100.158.712 |
| Chemical and physical data | |
| Formula | C17H25N3O2 |
| Molar mass | 303.406 g·mol−1 |
| 3D model (JSmol) | Interactive image |
| Solubility in water | Freely Soluble in water mg/mL (20 °C) |
| SMILES[hide]N#C[C@H]4N(C(=O)CNC13CC2CC(C1)CC(O)(C2)C3)CCC4 | |
| InChI[hide]InChI=1S/C17H25N3O2/c18-9-14-2-1-3-20(14)15(21)10-19-16-5-12-4-13(6-16)8-17(22,7-12)11-16/h12-14,19,22H,1-8,10-11H2/t12?,13?,14-,16?,17?/m0/s1 Key:SYOKIDBDQMKNDQ-XWTIBIIYSA-N |
////////VILDAGLIPTIN, LAF 237,NVP LAF 237, ビルダグリプチン , GALVUS, EQUA, NOVARTIS, DIABETES
OC12CC3CC(C1)CC(C3)(C2)NCC(=O)N1CCC[C@H]1C#N
Reference:
[1]. Japan, PMDA.
[2]. Drug@EMA, EMEA/H/C/000771 Galvus : EPAR – Scientific Discussion.
[3]. Postgrad. Med. J. 2008, 84, 524-531.
[4]. Diabetes Obes. Metab. 2011, 13, 7-18.
[5]. Diabetes Metab. 2012, 38, 89-101.
[6]. Formulary 2008, 43, 122-124, 131-134.
[7]. Br. J. Diabetes Vasc. Dis. 2008, 8, S10-S18.
[8]. Drugs 2011, 71, 1441-1467.
[9]. The relevance of off-target polypharmacology; John Wiley & Sons, Inc., 2012.
[10]. Int. J. Clin. Pract. Suppl. 2008, 62, 8-14.
[11]. Best Pract. Res. Clin. Endocrinol. Metab. 2009, 23, 479-486.



























































































![MS 2 spectrum of the [M þ H] þ ion (m/z 370) of imrecoxib (inset, full-scan mass spectrum).](http://www.researchgate.net/profile/Dafang_Zhong/publication/6930659/figure/fig4/AS:394580018122760@1471086616006/MS-2-spectrum-of-the-M-th-H-th-ion-m-z-370-of-imrecoxib-inset-full-scan-mass.png)




